Viral hemorrhagic fevers
Definition:
Viral hemorrhagic (hem-uh-RAJ-ik) fevers are infectious diseases that interfere with the blood's natural ability to clot. These diseases can also damage the walls of tiny blood vessels, making them leaky. The internal bleeding that results can range from relatively minor to life-threatening.
Some viral hemorrhagic fevers include:
Viral hemorrhagic fevers are spread by contact with infected animals, people or insects. No current treatment can cure viral hemorrhagic fevers, and immunizations exist for only a few types. Until additional vaccines are developed, the best approach is prevention.
Symptoms:
Signs and symptoms of viral hemorrhagic fevers vary by disease. In general, initial symptoms may include:
Severe cases of some types of viral hemorrhagic fevers may cause bleeding:
The best time to see a doctor is before you travel to a developing country to ensure you've received any available vaccinations and pre-travel advice for staying healthy. If you develop signs and symptoms once you return home, consider consulting a doctor who focuses on international medicine or infectious diseases. A specialist may be able to recognize and treat your illness faster. Be sure to let your doctor know what areas you've visited.
Causes:
The viruses that cause viral hemorrhagic fevers live naturally in a variety of animal and insect hosts — most commonly mosquitoes, ticks, rodents or bats.
Each of these hosts typically lives in a specific geographic area, so each particular disease usually occurs only where that virus's host normally lives. Some viral hemorrhagic fevers also can be transmitted from person to person.
How is it transmitted?
The route of transmission varies by specific virus. Some viral hemorrhagic fevers are spread by mosquito or tick bites. Others are transmitted by contact with infected blood or semen. A few varieties are breathed in if you're around infected rat feces or urine.
If you travel to an area where a particular hemorrhagic fever is common, you may become infected there and then develop symptoms after you return home
Complications:
Viral hemorrhagic fevers can damage your:
Treatments and drugs:
Medications
While no specific treatment exists for most viral hemorrhagic fevers, the antiviral drug ribavirin (Virazole, Rebetol) may help shorten the course of infection and prevent complications in some cases.
Therapy
Supportive care is essential. To prevent dehydration, you may need fluids to help maintain your balance of electrolytes — minerals that are critical to nerve and muscle function.
Surgical and other procedures
Some people may benefit from kidney dialysis, an artificial way of cleaning wastes from your blood when your kidneys fail.
Definition:
Viral hemorrhagic (hem-uh-RAJ-ik) fevers are infectious diseases that interfere with the blood's natural ability to clot. These diseases can also damage the walls of tiny blood vessels, making them leaky. The internal bleeding that results can range from relatively minor to life-threatening.
Some viral hemorrhagic fevers include:
- Dengue
- Ebola
- Lassa
- Marburg
- Yellow fever
Viral hemorrhagic fevers are spread by contact with infected animals, people or insects. No current treatment can cure viral hemorrhagic fevers, and immunizations exist for only a few types. Until additional vaccines are developed, the best approach is prevention.
Symptoms:
Signs and symptoms of viral hemorrhagic fevers vary by disease. In general, initial symptoms may include:
- High fever
- Fatigue
- Dizziness
- Muscle aches
- Weakness
Severe cases of some types of viral hemorrhagic fevers may cause bleeding:
- Under the skin
- In internal organs
- From the mouth, eyes or ears
- Shock
- Nervous system malfunctions
- Coma
- Delirium
- Seizures
- Kidney failure
The best time to see a doctor is before you travel to a developing country to ensure you've received any available vaccinations and pre-travel advice for staying healthy. If you develop signs and symptoms once you return home, consider consulting a doctor who focuses on international medicine or infectious diseases. A specialist may be able to recognize and treat your illness faster. Be sure to let your doctor know what areas you've visited.
Causes:
The viruses that cause viral hemorrhagic fevers live naturally in a variety of animal and insect hosts — most commonly mosquitoes, ticks, rodents or bats.
Each of these hosts typically lives in a specific geographic area, so each particular disease usually occurs only where that virus's host normally lives. Some viral hemorrhagic fevers also can be transmitted from person to person.
How is it transmitted?
The route of transmission varies by specific virus. Some viral hemorrhagic fevers are spread by mosquito or tick bites. Others are transmitted by contact with infected blood or semen. A few varieties are breathed in if you're around infected rat feces or urine.
If you travel to an area where a particular hemorrhagic fever is common, you may become infected there and then develop symptoms after you return home
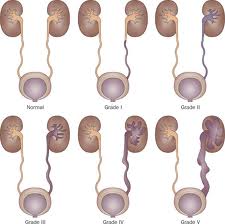
Complications:
Viral hemorrhagic fevers can damage your:
- Brain
- Eyes
- Heart
- Kidneys
- Liver
- Lungs
- Spleen
Treatments and drugs:
Medications
While no specific treatment exists for most viral hemorrhagic fevers, the antiviral drug ribavirin (Virazole, Rebetol) may help shorten the course of infection and prevent complications in some cases.
Therapy
Supportive care is essential. To prevent dehydration, you may need fluids to help maintain your balance of electrolytes — minerals that are critical to nerve and muscle function.
Surgical and other procedures
Some people may benefit from kidney dialysis, an artificial way of cleaning wastes from your blood when your kidneys fail.


.jpg)





.jpg)

.jpg)

.jpg)

.jpg)
.jpg)







.jpg)